Managing the emotional strain of Diabetes requires knowledge, good medical care, and emotional strength.

A handful of actionable behaviors and helpful tools can build your emotional strength and help you successfully manage both the physical and mental aspects of diabetes.
How Does Diabetes Affect Daily Life?
Diabetes is one of the few diseases that require round-the-clock attention and energy, taking a toll on patients mentally and physically. Why? Diabetes is more than just eating well, exercising, and checking your glucose. It affects almost everything in daily life and can be tiring to manage and control.
The emotional impact of the disease on patients' lives is real and often takes a back seat to the physical effects diabetes has on the body, even though it is equally as crucial to take care of the mental stresses it causes. Because while poor physical care can cause dangerous complications, the psychological burdens of diabetes can be just as threatening. It can cause burn-out, feelings of powerlessness, discouragement, worry, and depression, which your body reacts to. Additionally, these negative emotions can lead to you making poor lifestyle choices and interfere with your ability to take care of your body. Therefore, the best way to treat your diabetes is to realize the connection between the body and the mind and nurture them equally.
These tips address common concerns about diabetes-related stress and help you handle your emotions as well as your demanding self-care routines.
“I’m tired of the blame and shame.”
As with other health conditions, lack of information leads to misunderstanding and judgment about people living with diabetes. Stigma can be a major challenge for people with diabetes. In a 2013 research study about the social stigma surrounding diabetes, one woman said, "I call it the ‘blame and shame disease’ because I think that people get blamed and shamed and I think that makes it worse...they feel hopeless.” Diabetes stigma exists everywhere; it can occur in your family, school, workplace, and healthcare setting. The shame resulting from such widespread misinformation can prevent people from taking care of their physical and mental health.
Unfortunately, stigma does not go away on its own. It requires those who have knowledge and experience about diabetes to be willing to teach people about it and the struggles of living with the disease. Understandably, it can be challenging and vulnerable to share your own experiences and start a conversation with people who carry a stigma.
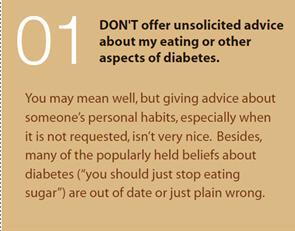
One way to make it easier is to use a diabetes etiquette card. The Behavioral Diabetes Institute developed these cards to help educate people in a lighthearted way. They’re polite and bring up important points. You can buy them on the BDI website or create them yourself! They can include what not to say to a person with diabetes, common misconceptions, facts, general information, appropriate ways to frame questions, and unbiased language when communicating about diabetes. Whenever you find yourself needing to explain why you can’t eat a particular food your friend really wants you to try or why you’re offended by someone calling you diabetic, hand them an etiquette card.
Another solution is to practice your responses to misleading information. That way, you can feel more comfortable correcting someone if you need to, and you can state it in a way they can understand. Starting these conversations about what diabetes really is and how it affects people can be instrumental to removing stigma and providing support instead of blame and shame.
“No one understands what I'm going through.”
A common problem among people struggling emotionally with diabetes is having feelings such as a lack of understanding, recognition, and emotional support. Your family and friends know that having diabetes is challenging but may not understand how it impacts you emotionally on a day-to-day basis. This feeling of loneliness can determine how you think and feel, handle stress, relate to others, and make choices. Therefore, having a plan for managing the emotional side of diabetes is just as important as a plan for your physical care.
Talking about diabetes and how the condition makes you feel is not always easy. It can be hard to find someone you think you can open up to, or it can make you feel like you are burdening people with your problems. However, offloading some of your difficulties has so many benefits, both for you and those close to you. You can start by incorporating practices such as support groups or family therapy into your life as part of your plan to focus on your emotions. These activities can make you feel less alone and more connected.
Diabetes can be tough on the whole family. In family therapy, you can learn to work together to manage your condition and how they can best support you. It can also be helpful to find a support group where you can connect with other people who understand firsthand what you’re going through. Thankfully there are many ways to do this. You can start with the government and nonprofit community groups hosted by the American Diabetes Association (ADA) and the Centers for Disease Control and Prevention (CDC). From there, you can get involved in Diabetes forums like Diabetes Daily and Social Media Pages such as Healthline’s Facebook page Living with Diabetes. The benefits of support groups online and in-person are endless. Whether you join for helpful tips or friendship, interacting with people who share a similar experience can be a powerful resource for improving the quality of your life and taking control of your diabetes.
“I want to take care of myself, but it’s too much work.”
Managing diabetes is highly complex. People who have diabetes deal with the complications of the disease, the anxiety, and the strictly regulated lifestyle associated with diabetes—24 hours a day, 365 days a year. Successful diabetes management requires people to adopt new habits relating to medication adherence, glucose monitoring, food, and exercise. So, understandably it is difficult to feel successful in their diabetes management without feeling burdened by it. This feeling may also cause people to feel isolated from others who don’t have to worry about these things. For some, these overwhelming feelings start to affect their behavior. They either ignore what they must do to keep their diabetes under control or work hard to manage their condition and still feel a sense of failure.
Diabetes does change your life, but it doesn't have to stand in the way of you living the life you want. Many people have found that having a daily routine helps them manage their diabetes better. Together, a daily routine and various forms of stress reduction, like meditation, yoga, breathing techniques, massages, self-love, and keeping up motivation, can make you feel more balanced. Your day-to-day diabetes routine should be specific to your situation and needs, such as what medications you take. It can include healthy habits like checking and logging your blood sugar when you wake up, planning healthy meals throughout the day, and taking a walk after meals. It is also helpful to build time for yourself into your routine. For example, sitting quietly for 15 minutes or setting an evening aside for a long bath can help you relax.
According to Charles Duhigg, the author of The Power of Habit, there is power in creating habits. The reason is that habits create neurological cravings that reward certain behaviors with “pleasure” chemicals in the brain. Building a routine is an excellent way to give your habits the space and structure to grow, so the new behavior becomes less of a decision and more automatic. When you have diabetes, it can seem like you’re juggling a lot in a day but maintaining an effective routine maximizes your ability to thrive without feeling overwhelmed.
“I feel like I can’t enjoy food anymore.”
Those diagnosed with diabetes experience a distinctive and strict emphasis placed on food types and amounts. This hyper-focus on food, eating, and weight is often a contributing factor in the unhealthy relationship with food and the development of an eating disorder. Those with diabetes may begin to see foods as “good” or “bad” (based on blood glucose management). Diabetes is also often a notable life event and stressor. A significant shift like this can lead individuals to develop an eating disorder to gain control and feel as if they are “successful” in treating their illness.
Because there is such a big focus on food and eating, it can be hard to enjoy a meal without thinking about what this means for your body. You don't have to give up your favorite meals just because you have diabetes, but you need to know how your choices affect your blood sugar. Registered Dietitian Brenda Manzanarez and Dr. Cynthia Muñoz recommend rethinking the role of the food on your plate. Instead of thinking about food as either "good" or "bad" or dieting, adopt a nonjudgmental view of food and eat foods that provide energy and fuel to your body. While it is essential to eat foods to ensure you're getting the vitamins and minerals your body needs, eat the foods you like!
It also might be helpful to seek the assistance of a diabetes educator or dietitian. They can teach you how to count carbs, read food labels, and size up portions in a healthy way. Those skills will let you control your diabetes and keep your taste buds happy at the same time.
“I’m so afraid of the complications from hypoglycemia.”
Hypoglycemia is one of the most common complications of diabetes, especially for people with type 1. Therefore, fear of hypoglycemia is a commonly reported problem for people with diabetes and their families. Hypoglycemia is the medical term for low blood glucose or low blood sugar levels. Symptoms can include dizziness, confusion, hunger, or irritability. In some cases, there can be no symptoms at all. The fear of hypoglycemia can be one of the barriers to better glycemic management. This is because some patients prefer to keep high blood glucose levels to avoid hypoglycemia. However, this increases the risk of developing complications which can be very dangerous to your health and potentially fatal.
Of course, having fear is normal, but you don't want to let it get in the way of your decision-making or your daily diabetes management. To overcome the fear of hypoglycemia, start logging your hypos so you can learn your unique alarm bells. Everyone has their warning signs that are their body's way of telling them that they are low. Start to pay attention to what goes on with your body when you get low. It may be a physical symptom (like tingling in a particular part of your body, sweating, headache, or heart palpitations) or a mental symptom (like nervousness, moodiness, or confusion). Sometimes the fear of hypoglycemia is too debilitating, and you may have trouble overcoming it by yourself. In this case, you may want to seek treatment from a mental health care provider who specializes in diabetes and can help you cope with this challenge.
“It’s too difficult to travel with diabetes.”
Although you may not feel comfortable traveling at this time due to Covid-19, looking to a future when it is safe to do so, for many, Diabetes presents a big problem. While Diabetes can make travel more challenging, it doesn’t have to stop you from taking the trips you want. Whether you plan a tropical vacation to the beach, backpacking in South America, or a business trip, the key to a good trip is to be over-prepared. Being prepared does require planning, but the more you plan, the more you’ll be able to relax and enjoy the experience. Many people have concerns about traveling to new places because it gets you out of your routine, but instead of letting that hold you back, think of it as part of the fun. As long as you plan carefully and pack thoughtfully, you can travel safely.

Ellen Lindner / Verywell
Here are a few ways you can prepare for your trip:
The ADA recommends talking with your doctor to adjust and ensure you have medication to last the duration of your stay.
You can get a medical ID bracelet that states you have diabetes and any other health conditions.
When you visit a country where English is not the primary language, it may be helpful to learn phrases in the native language. These phrases should include statements like “I have diabetes” and “can I please have some orange juice?”
Create a checklist to guarantee you do not leave home without a doctor's letter and prescriptions, snacks and glucose tablets, and extra insulin and diabetes medicines.
There are tons of suggestions for what to bring with you when you leave home online as well. For more detailed travel tips before, during, and after travel, visit the CDC’s recommendations.
“What's the point of doing all the so-called right things, when I'm going to have complications either way.”
Too many people still don’t know the benefits of proper care and feel doomed to suffer from complications. They are unable to overcome obstacles to manage their diabetes and end up suffering from hopelessness and depression. These feelings of fear get in the way of diabetes self-care.
This obstruction presents itself in a few ways:
When people only focus on avoiding complications instead of accurately managing their diabetes
When people avoid getting the care they need because they are afraid of the result
When people neglect to take care of themselves at all because they’ve lost hope
The most effective way to combat this type of thinking is to fight fear with knowledge and understand the benefits of good care. After all, it is not diabetes that causes serious problems rather poorly managed diabetes. Think about your diabetes as a whole instead of going down the rabbit hole trying to avoid any particular complication.
Stay in charge of your health by focusing on everything that goes into managing blood glucose levels, things like eating healthfully, exercising, and managing stress. It also means using medical devices and technology available to you and getting regular foot, dental, and eye exams. The practices they use today may not be the same tomorrow as our understanding of diabetes has improved dramatically in our lifetimes and will keep progressing. Even still, there is no single straight line of care.
One of the best things you can do to prevent feeling defeated is to create a reliable team who can support you and understands what you’re going through. This team can include a podiatrist, ophthalmologist, endocrinologist, diabetic nurse, diabetic educator, dermatologist, and therapist. These are all people who are experts on the most effective way to manage your diabetes, avoid complications, and restore hope in living a long, vibrant life.
SOURCES:
https://diatribe.org/diabetes-stigma-everywhere-you-can-do-something-about-it
https://www.cdc.gov/diabetes/managing/mental-health.html
https://www.everydayhealth.com/hs/diabetes/healthy-daily-routine-for-diabetes/
https://beyondtype1.org/overcoming-foh-fear-of-hypoglycemia/
https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-management/art-20047963
https://type2diabetes.com/living/fear-complications-understand